A few days ago, I had my 10th surgery. This one was different as opposed to the previous nine. For the first time I was permitted to wear my pump during the procedure.
So how did it go?
This was a fairly quick, laparoscopic abdominal surgery. Patients without comorbidities are usually back home in a few hours. Since I have adrenal insufficiency and some signs of pheochromocytoma, they did keep me a little longer as a precaution.
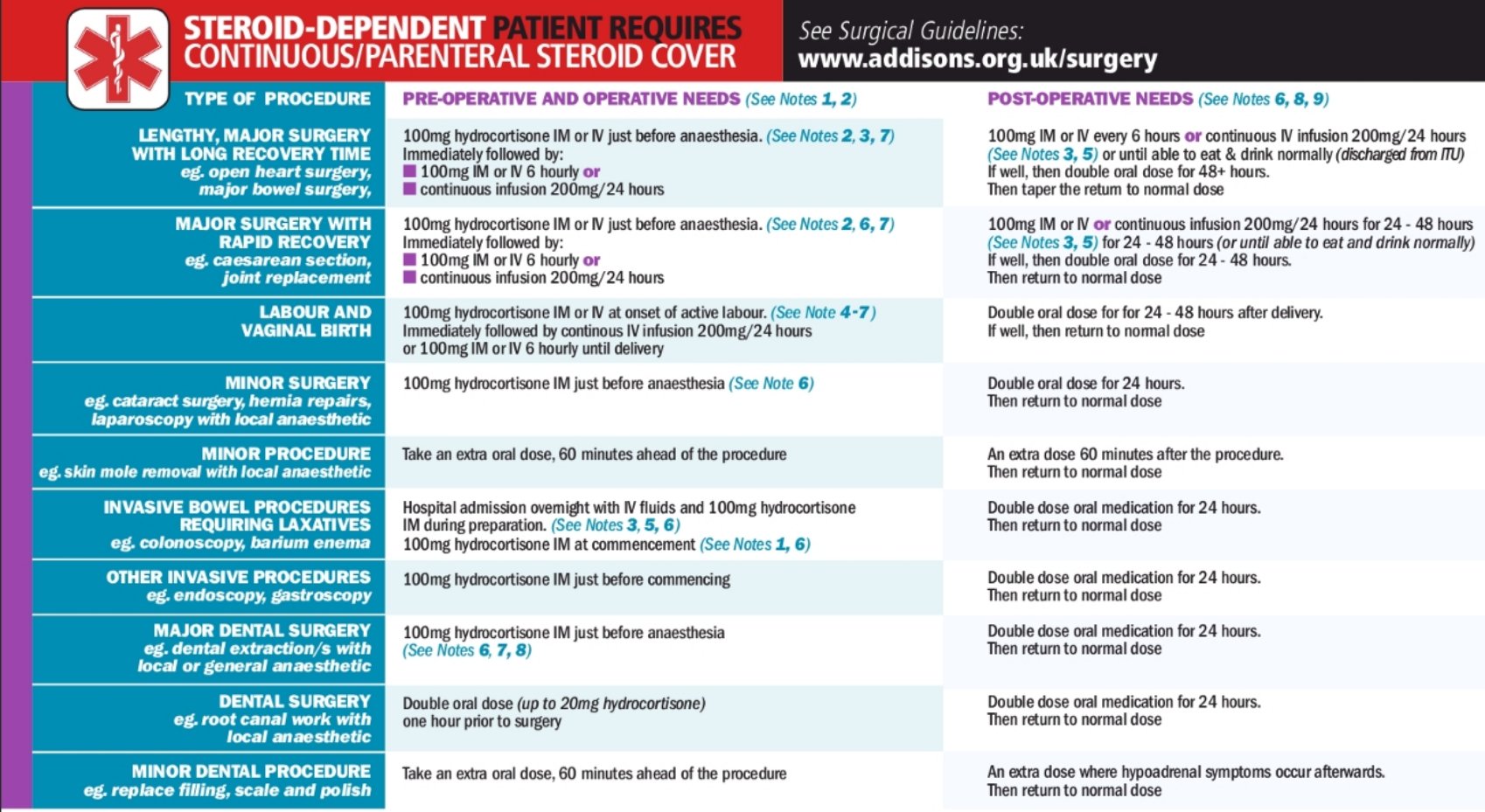
Speaking of precautions, if you have adrenal insufficiency you MUST speak to your surgeon, endocrinologist and anesthesiologist about your steroid plan for surgery. Everyone needs to be on the same page. I can’t tell you how many times I’ve heard adrenal insufficient patients say, “oh the anesthesiologist knows what to do” DO NOT EVER MAKE THAT ASSUMPTION! They do tend to keep solu-cortef in the operating room, but that doesn’t mean they will dose it correctly. Some anesthesiologists deviate from the standard of care and come up with their own plan using less steroid. They think they’re doing you a favor, when really they are unknowingly endangering your life and hindering your recovery. DO NOT LEAVE THIS UP TO CHANCE! Make sure you’re on the same page!
As soon as surgery was mentioned, I made my concerns clear. I knew there would need to be special precautions because of the risk of adrenal crisis or hypertensive episodes due to pheo. I spoke to my surgeon and endo about this as well as two anesthesiologists. I had to have more tests than the norm in order to be cleared for surgery. I had to have any possible pheo activity blocked by taking blood pressure medication for a couple months. At this hospital they don’t assign an anesthesiologist until the night before the procedure. This makes communication a challenge, but by the time I actually met her, pretty much everyone including the nurses had already heard about my steroid plan and pheo concerns. When I discussed it with her, she had already heard my plan and was thankfully in agreement. I would receive 100mg of solu-cortef before and after the procedure and keep my pump running.
This is where I made a mistake. I planned on running a straight 10mg/hr during the procedure. However I forgot to program that profile into my pump. I programmed it in pre-op and realized my settings only allowed me to go as high as 8mg/hr. I didn’t want to edit my settings at the last minute, so I programmed 8mg/hr. That would have worked just fine except I FORGOT TO SWITCH OVER TO THAT PROFILE. Yes, it is all well and good to program a profile, but you have to actually “run” said profile for it to work. Oops! So during the procedure I was running my normal every day basal program of 30.2mg/daily. 🤦♀️
I woke up being wheeled into recovery. My abdomen hurt so bad. They gave me IV pain medication, but the relief began to fade after a couple minutes. They gave me another dose. Then I watched the nurse give me 100mg of solu-cortef. 15 minutes later I was moved to a regular room. That’s when I realized there was a problem. The IV pain meds had worn off already. My pain was uncontrolled. I felt nauseous, but the nurse would not give me any oral pain medication until I ate something. I had a couple spoonfuls of pudding and felt sick. I was given IV zofran with minimal effect. Still sick. Every IV medication I’d been given seemed to metabolize way too fast. This has always been the case for me, and it’s the main reason I had to switch to the cortisol pump to begin with.
There’s a familiar and unpleasant feeling I get when my cortisol isn’t sufficient. It’s an uneasy, almost panic feeling where I’m keenly aware that something isn’t right and I’m increasingly desperate to find relief or escape. It’s more like a primal instinct, “Something is wrong, help me!” I’ve unfortunately felt this enough times to realize it was cortisol related. I realized then my pump was still set on the measley 30mg profile. I immediately switched it to the 8mg/hr profile that I had programmed in pre-OP. The problem is it takes a while for pump rates to build your blood cortisol level. For whatever reason my body did not keep those 100mg IV solu-cortef boluses in my system very long. So I had to suffer while my rates caught up. Meanwhile the nurse had given me a couple doses of pain pills, and IV phenergan. Phenergan only helped the nausea for 5 minutes or so, but thankfully it made me extremely sleepy. I was able to sleep through the misery and give my pump some time to do its thing. A few hours later the nurse came in to check on me, by then the pain meds were working and my pump was kicking butt. I was still pretty knocked out from the phenergan, but I felt well enough to get dressed and go home. My nausea was gone and my appetite had returned. Yay for proper steroid dosing!
Friends, I can’t tell you enough how much sufficient steroid dosing will make or break a situation. Especially a high stakes situation like a surgery. It’s amazing how fast I went from utter misery in the hospital, to eating a sandwich at home. Steroids ya’ll! They’re a big deal! I stepped down to my 84mg/daily “sick” basal profile and kept it there until late evening. Note: your ability to lower your stress dose will be a case by case situation and depends on what type of surgery you had, how long it was and how invasive it was. Pain control is a major factor. Stay on top of your pain medication schedule. Do not let your meds lapse or try to suffer through it. This will increase your body’s cortisol need, hinder your ability to taper your steroid dose, and potentially prolong your recovery. You need sufficient steroid dosing to get pain under control and you need your pain meds to keep your cortisol need under control. They go hand in hand, don’t skimp on one or the other.
Quick PSA: When you’re running high rates. YOU WILL need to change your inset more often. Pumping during surgery and recovery sounds pretty convenient compared to stress dosing with pills, and it was, but what I did not mention is all the stress that kind of volume puts on an infusion site. My site was leaking by bed time, which I totally expected to happen. This is EVEN MORE true if you run 2:1 dilution ratio in your pump because you are pumping twice the volume than those on 1:1 ratio. So yes, stress dosing and sick dosing with the pump is easier and more effective than pills, but DO NOT NEGLECT YOUR SITE! Don’t wait for it to start leaking either! When you’re ill/recovering your body needs cortisol the most, this is not the time to wait around for a site failure! I’ve changed my site DAILY while recovering from this procedure.
I’ve had 2 previous surgeries as a pumper, but the medical teams for those procedures were not familiar with, or keen on the idea of pumping during surgery, and I didn’t push them for it. After my experience pumping during this latest procedure, I am going to push for my pump every time. Infection risk is minimal, it’s less than that of the actual surgery itself. The continuous delivery of the pump is ideal for recovery and superior to IV bolusing dosing only, especially since hospitals seem to think bolusing once every 8-12 hours is going to work fine. Its miserable. Continuous delivery is where it’s at! One day they’ll get with the times I hope.
At the time of writing it’s been nearly 48 hours since my surgery. I’m back on my normal profile plus a 200% increase (double dosing). My energy is good and my pain is well controlled as long as I keep up the pain medication schedule. My biggest problem at the moment is remembering not to over do it. I’m tempted to clean house, go on a walk, etc, and I dont feel like resting like I should. Steroid dosing makes a world of difference, and the pump makes this a much smoother experience. Just don’t neglect your infusion site or your pain meds! Happy healing friends!
❤Michelle